Volume 80, Issue 2
Displaying 1-50 of 54 articles from this issue
-
2012 Volume 80 Issue 2 Pages 1-16
Published: 2012
Released on J-STAGE: May 01, 2013
DOIhttps://njjn-jsjc-gov-cn-s-1416.res.gxlib.org.cn:443/rwt/1416/https/MSYXTLUQPJUB/10.11641/pde.80.2_1Download PDF (8575K)
-
2012 Volume 80 Issue 2 Pages 37-41
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (407K) -
2012 Volume 80 Issue 2 Pages 42-46
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (289K) -
2012 Volume 80 Issue 2 Pages 47-51
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (329K) -
2012 Volume 80 Issue 2 Pages 52-54
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (293K) -
The combination of short and long type hemoclips therapy was effective for hemorrhagic gastric ulcer2012 Volume 80 Issue 2 Pages 55-58
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (409K) -
“Bridge to surgery” stenting and laparoscopic colorectal resection for obstructive colorectal cancer2012 Volume 80 Issue 2 Pages 59-62
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (500K) -
2012 Volume 80 Issue 2 Pages 63-65
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (346K) -
2012 Volume 80 Issue 2 Pages 66-67
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (359K) -
2012 Volume 80 Issue 2 Pages 68-69
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (261K)
-
2012 Volume 80 Issue 2 Pages 70-71
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (317K) -
2012 Volume 80 Issue 2 Pages 72-73
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (633K) -
2012 Volume 80 Issue 2 Pages 74-75
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (190K) -
2012 Volume 80 Issue 2 Pages 76-77
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (238K) -
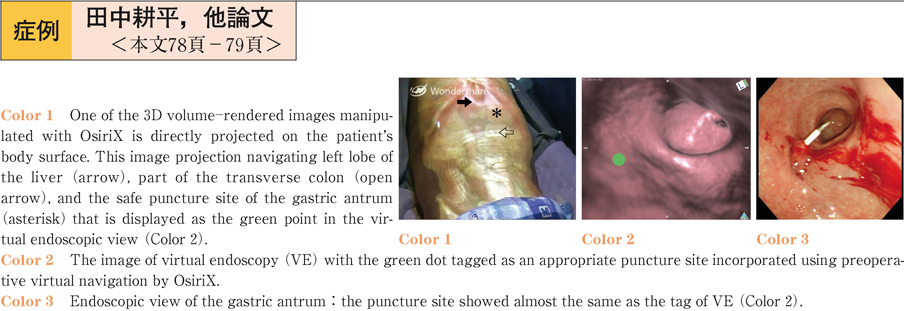
2012 Volume 80 Issue 2 Pages 78-79
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (280K) -
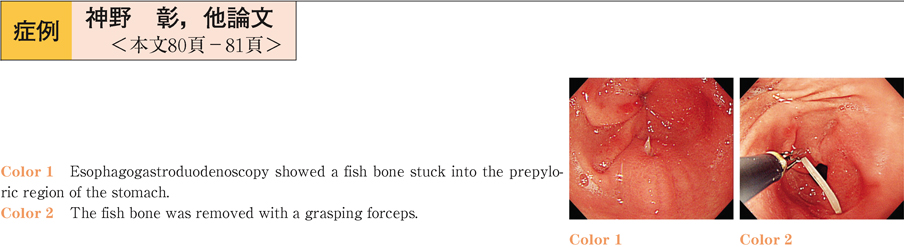
2012 Volume 80 Issue 2 Pages 80-81
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (297K) -
2012 Volume 80 Issue 2 Pages 82-83
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (273K) -
2012 Volume 80 Issue 2 Pages 84-85
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (561K) -
2012 Volume 80 Issue 2 Pages 86-87
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (279K) -
2012 Volume 80 Issue 2 Pages 88-89
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (339K) -
2012 Volume 80 Issue 2 Pages 90-91
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (584K) -
2012 Volume 80 Issue 2 Pages 92-93
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (456K) -
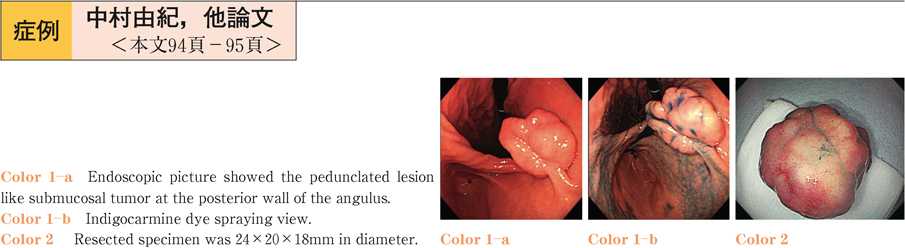
2012 Volume 80 Issue 2 Pages 94-95
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (490K) -
2012 Volume 80 Issue 2 Pages 96-97
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (455K) -
2012 Volume 80 Issue 2 Pages 98-99
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (249K) -
2012 Volume 80 Issue 2 Pages 100-101
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (343K) -
2012 Volume 80 Issue 2 Pages 102-103
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (243K) -
2012 Volume 80 Issue 2 Pages 104-105
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (351K) -
2012 Volume 80 Issue 2 Pages 106-107
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (487K) -
2012 Volume 80 Issue 2 Pages 108-109
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (590K) -
2012 Volume 80 Issue 2 Pages 110-111
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (469K) -
2012 Volume 80 Issue 2 Pages 112-113
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (365K) -
2012 Volume 80 Issue 2 Pages 114-115
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (235K) -
2012 Volume 80 Issue 2 Pages 116-117
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (402K) -
2012 Volume 80 Issue 2 Pages 118-119
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (272K) -
2012 Volume 80 Issue 2 Pages 120-121
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (311K) -
2012 Volume 80 Issue 2 Pages 122-123
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (744K) -
2012 Volume 80 Issue 2 Pages 124-125
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (219K) -
2012 Volume 80 Issue 2 Pages 126-127
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (304K) -
2012 Volume 80 Issue 2 Pages 128-129
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (387K) -
2012 Volume 80 Issue 2 Pages 130-131
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (515K) -
2012 Volume 80 Issue 2 Pages 132-133
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (518K) -
2012 Volume 80 Issue 2 Pages 134-135
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (285K) -
2012 Volume 80 Issue 2 Pages 136-137
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (258K) -
2012 Volume 80 Issue 2 Pages 138-139
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (511K) -
2012 Volume 80 Issue 2 Pages 140-141
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (420K) -
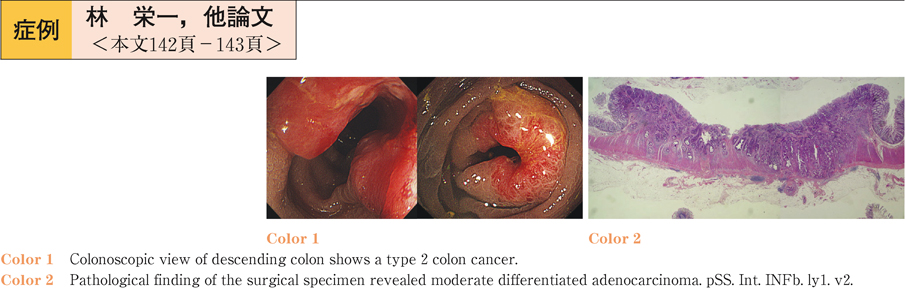
2012 Volume 80 Issue 2 Pages 142-143
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (291K) -
2012 Volume 80 Issue 2 Pages 144-145
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (351K) -
2012 Volume 80 Issue 2 Pages 146-147
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (401K) -
2012 Volume 80 Issue 2 Pages 148-149
Published: June 10, 2012
Released on J-STAGE: May 01, 2013
Download PDF (396K)