Volume 58, Issue 2
Displaying 1-44 of 44 articles from this issue
- |<
- <
- 1
- >
- >|
-
2001 Volume 58 Issue 2 Pages 1-10
Published: 2001
Released on J-STAGE: May 31, 2014
DOIhttps://njjn-jsjc-gov-cn-s-1416.res.gxlib.org.cn:443/rwt/1416/https/MSYXTLUQPJUB/10.11641/pde.58.2_1Download PDF (9259K)
Technology and instrument
-
2001 Volume 58 Issue 2 Pages 24-26
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (333K)
Clinical study
-
2001 Volume 58 Issue 2 Pages 28-32
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1510K) -
2001 Volume 58 Issue 2 Pages 34-38
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1309K) -
2001 Volume 58 Issue 2 Pages 40-43
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (474K) -
2001 Volume 58 Issue 2 Pages 44-48
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (3287K) -
2001 Volume 58 Issue 2 Pages 50-54
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (3354K)
Case report
-
2001 Volume 58 Issue 2 Pages 56-59
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (2001K) -
2001 Volume 58 Issue 2 Pages 60-63
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (432K) -
2001 Volume 58 Issue 2 Pages 64-67
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1095K) -
2001 Volume 58 Issue 2 Pages 70-71
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (213K) -
2001 Volume 58 Issue 2 Pages 72-73
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1433K) -
2001 Volume 58 Issue 2 Pages 74-75
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1193K) -
2001 Volume 58 Issue 2 Pages 76-77
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1240K) -
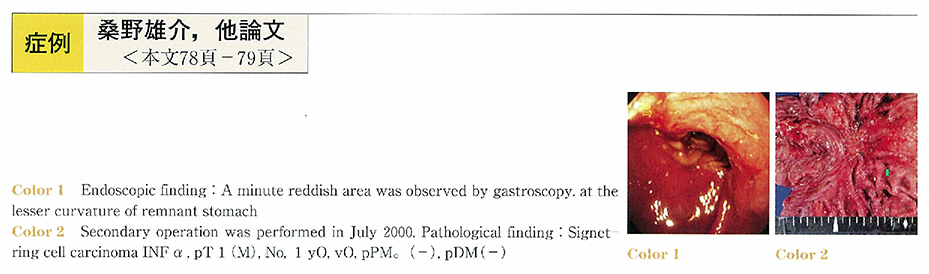
2001 Volume 58 Issue 2 Pages 78-79
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1223K) -
2001 Volume 58 Issue 2 Pages 80-81
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (843K) -
2001 Volume 58 Issue 2 Pages 82-83
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (901K) -
2001 Volume 58 Issue 2 Pages 84-85
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1240K) -
2001 Volume 58 Issue 2 Pages 86-87
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (923K) -
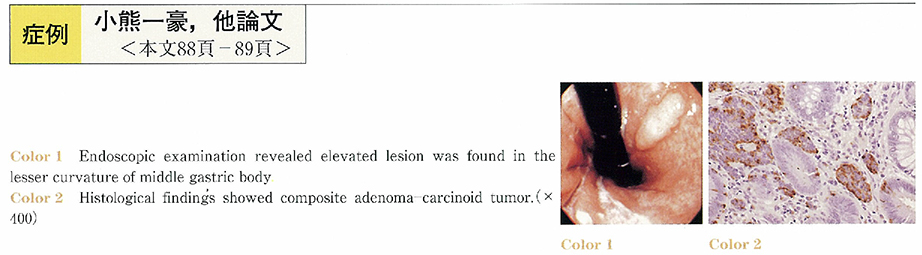
2001 Volume 58 Issue 2 Pages 88-89
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (881K) -
2001 Volume 58 Issue 2 Pages 90-91
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (907K) -
2001 Volume 58 Issue 2 Pages 92-93
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (921K) -
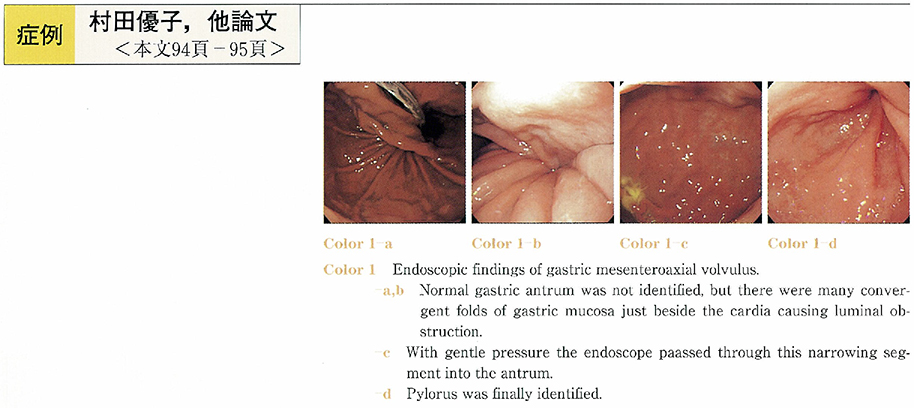
2001 Volume 58 Issue 2 Pages 94-95
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (601K) -
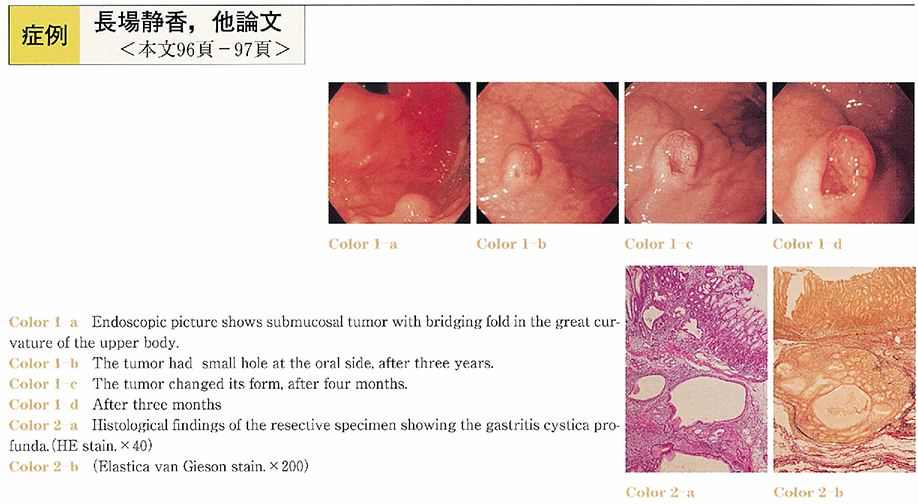
2001 Volume 58 Issue 2 Pages 96-97
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1293K) -
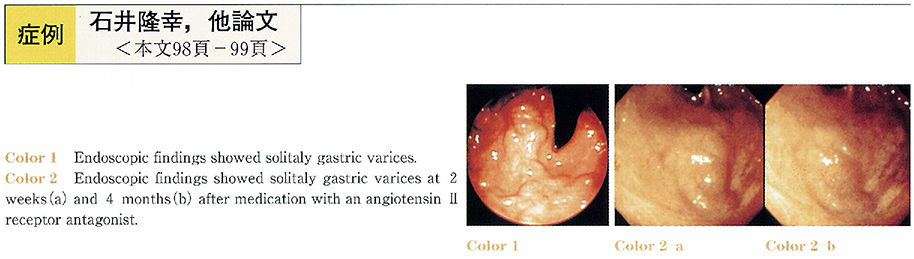
2001 Volume 58 Issue 2 Pages 98-99
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (967K) -
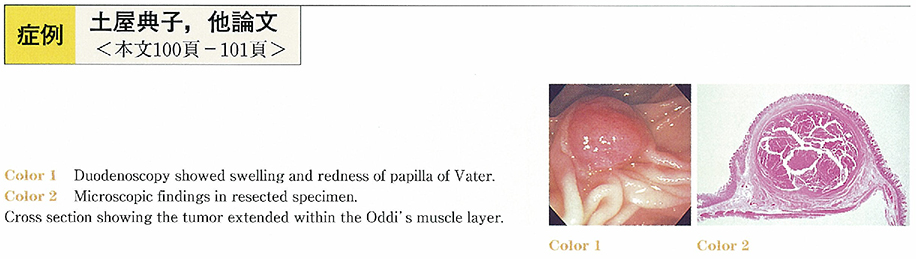
2001 Volume 58 Issue 2 Pages 100-101
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (777K) -
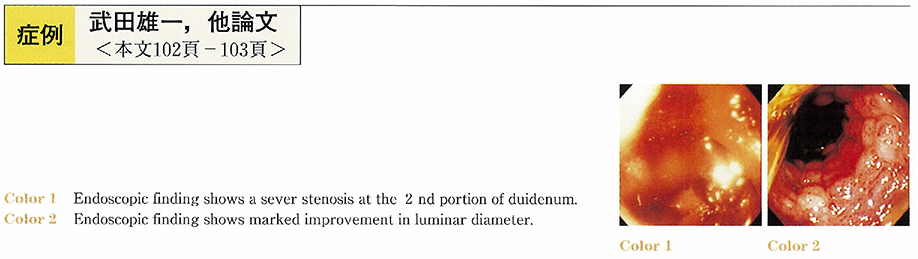
2001 Volume 58 Issue 2 Pages 102-103
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1524K) -
2001 Volume 58 Issue 2 Pages 104-105
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (675K) -
2001 Volume 58 Issue 2 Pages 106-107
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (258K) -
2001 Volume 58 Issue 2 Pages 108-109
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (759K) -
2001 Volume 58 Issue 2 Pages 110-111
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (715K) -
2001 Volume 58 Issue 2 Pages 112-113
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (310K) -
2001 Volume 58 Issue 2 Pages 114-115
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1245K) -
2001 Volume 58 Issue 2 Pages 116-117
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (570K) -
2001 Volume 58 Issue 2 Pages 118-119
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (206K) -
2001 Volume 58 Issue 2 Pages 120-121
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (483K) -
2001 Volume 58 Issue 2 Pages 122-123
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (241K) -
2001 Volume 58 Issue 2 Pages 124-125
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (703K) -
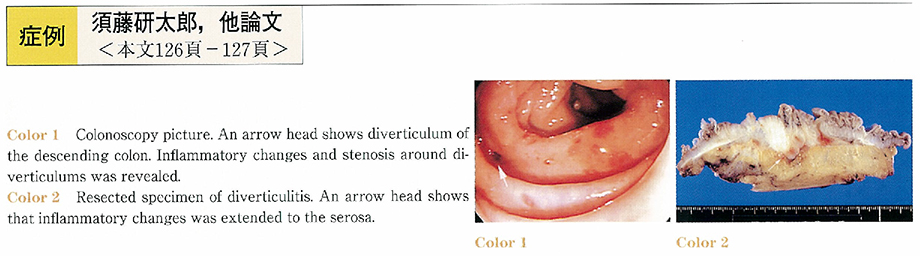
2001 Volume 58 Issue 2 Pages 126-127
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1103K) -
2001 Volume 58 Issue 2 Pages 128-129
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1213K) -
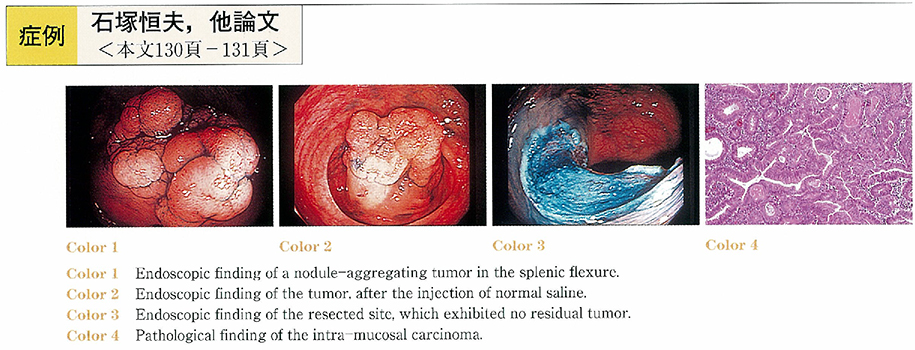
2001 Volume 58 Issue 2 Pages 130-131
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (622K) -
2001 Volume 58 Issue 2 Pages 132-133
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1449K) -
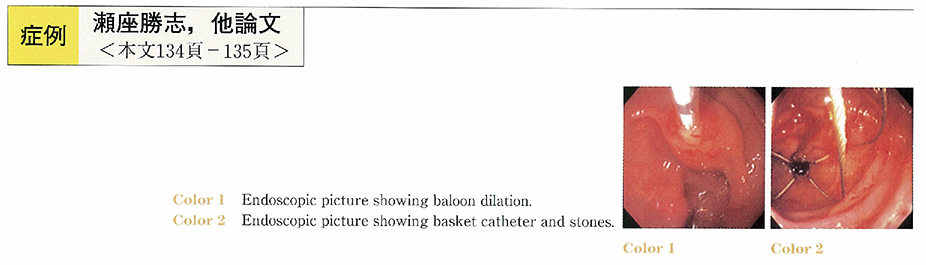
2001 Volume 58 Issue 2 Pages 134-135
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (1048K) -
2001 Volume 58 Issue 2 Pages 136-137
Published: June 15, 2001
Released on J-STAGE: May 31, 2014
Download PDF (934K)
- |<
- <
- 1
- >
- >|